MBC Care in the Middle of Nowhere
In the US, the majority of the country is considered rural. Researchers and policy officials employ many definitions to distinguish rural from urban areas, using rural-urban classifications adopted by NCI. An estimated 15% of the U.S. population and approximately 74% of the area is considered rural.
Residents of rural areas face serious challenges related to socioeconomic disadvantages, limited access to quality healthcare, long travel times, and low recruitment to clinical trials, all of which affect quality of care and health outcomes. Health disparities are exacerbated by the lack of health insurance, shortage of primary care physicians, oncologists and other cancer care specialists. Moreover, largely because of systematic marginalization (eg, historical segregation, and immigration laws), higher cancer incidence and mortality are observed in racial and ethnical minoritized groups. Collectively, these and other factors are associated with delayed cancer detection, more severe disease outcomes, and increased cancer mortality.
Rural areas often have fewer primary and specialty care physicians as well as fewer home- and community-based service providers compared to urban areas
Although an estimated 17%-20% of the U.S. population lives in rural areas, only 3% of medical oncologists practice in rural communities, and over 70% of counties in the U.S. do not have medical oncologists.
A recent study by the Centers for Disease Control and Prevention (CDC) reported that in the most recent period for which the data were available, rural counties had lower cancer incidence rates but higher death rates for all cancer sites combined. In addition, the study showed that the differences in death rates between rural and urban areas are increasing over time.
Stephanie Walker and Martha Carlson, this episode’s co-hosts and producers, take a closer and more intimate look at how geographical location, age, and ethnicity affect healthcare and quality of life. They speak with four women who share how their location in rural and remote areas impact the decisions on their care.
First, they interview Dr. Denise Belle. Dr. Belle serves as the Development Director with Rural Health Group, Inc. and has been a public health professional for 20+ years . Her research focuses on Black women living in rural, isolated areas and finding ways to cope with breast cancer.
Past episodes featuring non-profits which are serving rural communities:
Meet the Guests of the Episode
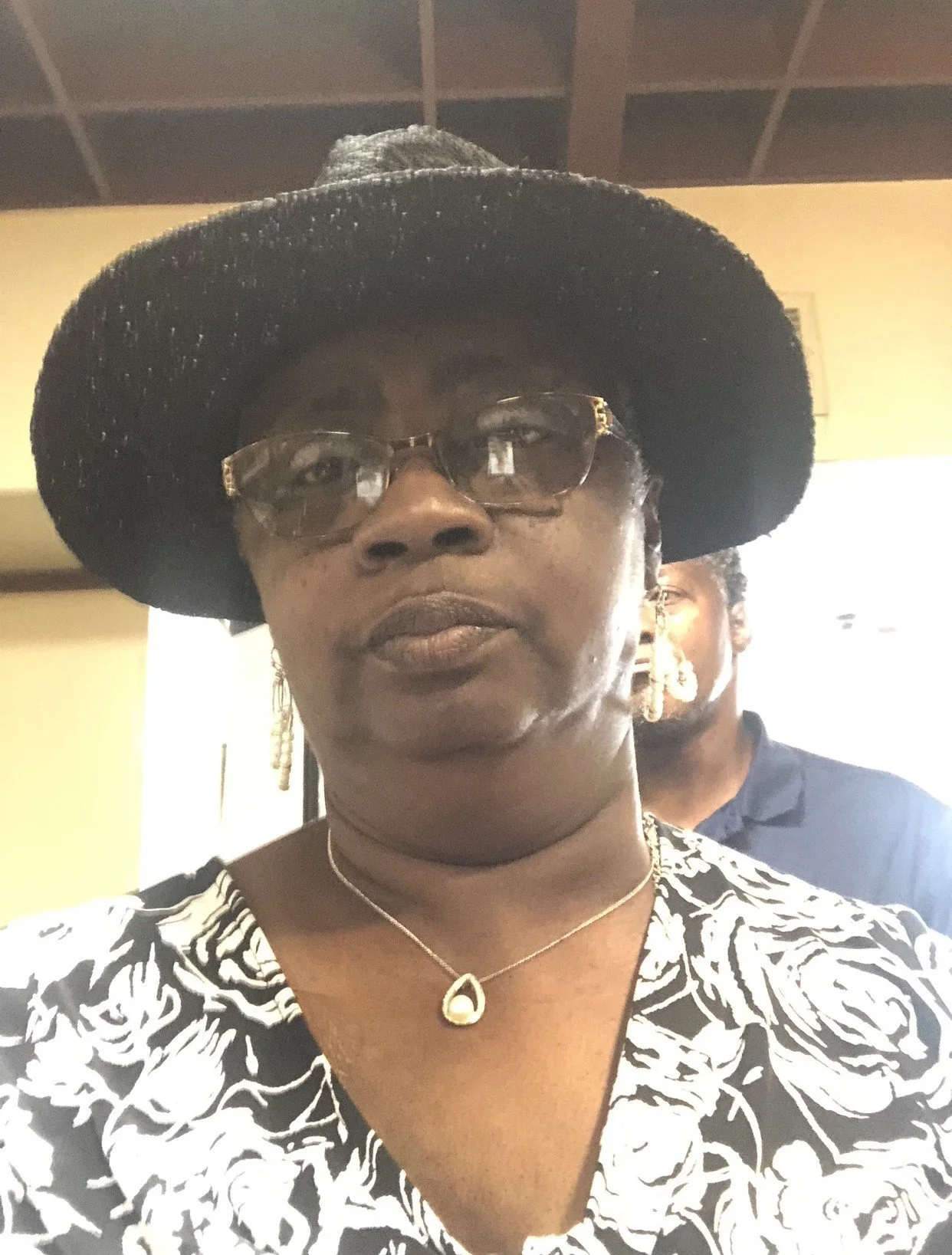
Evelyn Sharpe
Evelyn was initially diagnosed with early stage breast cancer in February of 2014, followed by a recurrence in February of 2019. She then had metastasis to the right side of her brain in March of 2023. She is currently receiving chemotherapy and will receive radiation again for a spot on the left side of her brain. Although she is going through tough times, her faith in God and love of life provides her the strength to get through, one day at a time.
Kristin Kilmer
Kristin is a wife and mother who works full-time leading communications and outreach for the South Dakota Department of Human Services while juggling treatments for metastatic breast cancer. Her start in advocacy began when she was diagnosed with Stage IIB breast cancer in 2011. Kristin pursued participation in a clinical trial as she believes research is the only way we will be able to successfully treat breast cancer in the future. After she was diagnosed with metastatic breast cancer in 2015, her interest in research advocacy increased. Due to a lack of options and support in her rural location, she currently drives nearly 800 miles every six weeks to meet with her oncology team and receive treatment. Kristin has spoken with numerous media outlets, including Cancer Today and Kaiser Health News, which led to a front-page feature in USA Today about the promise and limitations of precision medicine and the need for increased research funding. Kristin also participated in Living Beyond Breast Cancer’s Hear My Voice (HMV) Program in 2017 and in National Breast Cancer Coalition’s Project LEAD in June 2019.
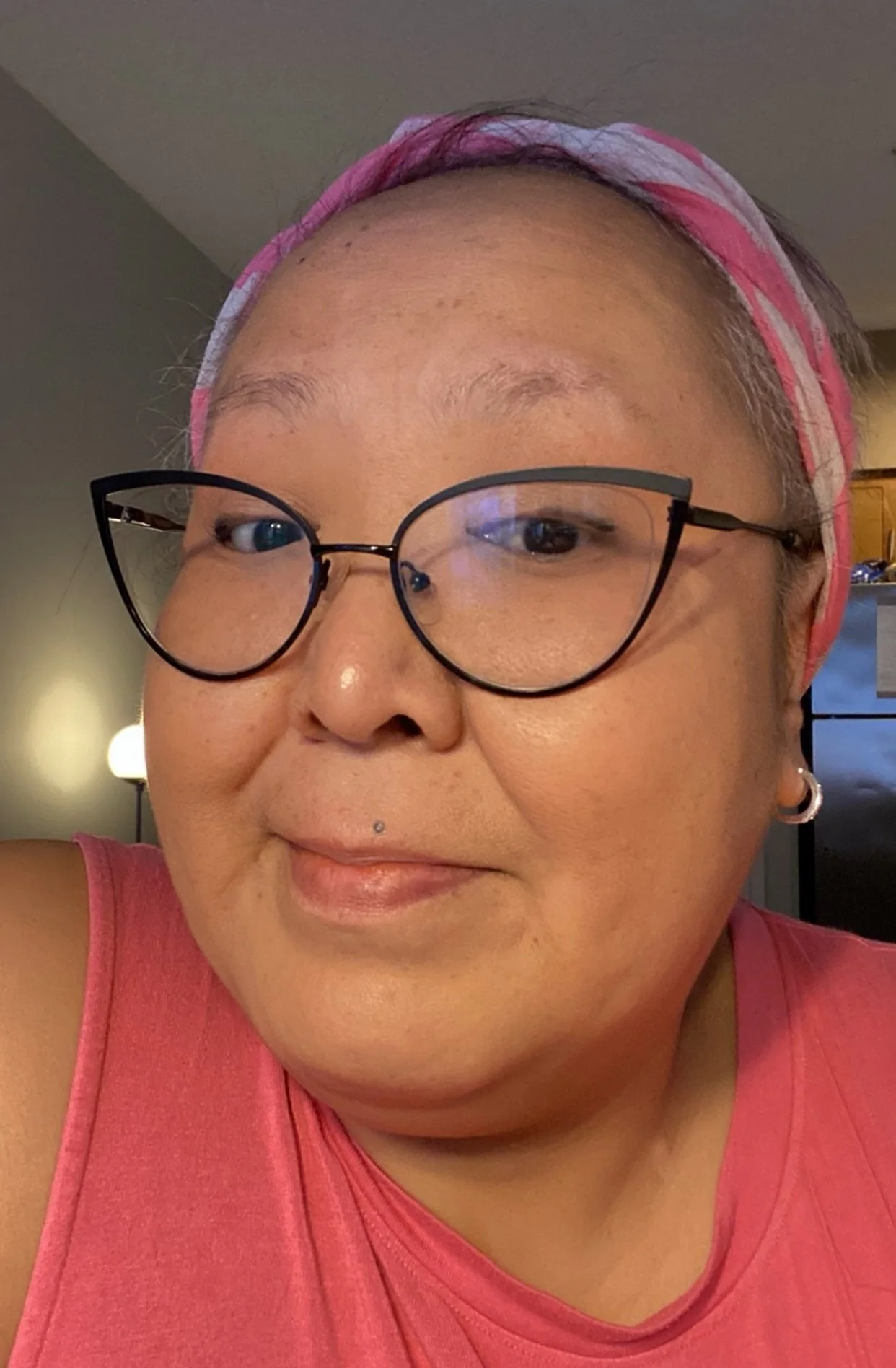
Mina Eningowuk
Mina, an Inupiaq from the Native Village of Shishmaref, Alaska, has had a remarkable journey. With a passion for working with children, Mina dedicated 13 years as an educational aide in elementary education. This experience allowed Mina to make a positive impact on the lives of many young learners.
Mina was diagnosed with stage 4 Invasive Lobular Carcinoma in February of 2018 and shares har diagnosis with family, friends and other MBC patients through Facebook support groups. Despite facing the challenges of stage 4 Invasive Lobular Carcinoma, Mina's strength and resilience shine through.
Veronica Fisher
Veronica is currently 54 years old and has been living with metastatic breast cancer for the past 9 years. In 2020, she completed advocacy training for Living Beyond Breast Cancer.
Denise Bell, PhD, MPH
Dr. Belle serves as the Development Director with Rural Health Group, Inc. Her role entails grants and relationship management, serving on various committees/coalitions, and is the organization’s community health center/research advocate. Dr. Belle has been a public health professional for 20+ years . Her research focuses on Black women living in rural, isolated areas and finding ways to cope with breast cancer. She has passion for minority rural communities. She would like to see more representation of minorities in clinical trials, research studies, and their voices included in the scientific literature. In addition, she desires meaningful research, equity – all aspects of life (income, environment, health care, etc.), and social change. In her spare time she cycles, gardens, loves spending time with her Mom and fur babies (two dogs), and is currently training for her first triathlon.
You can find her on LinkedIn.










Roberta Lombardi wanted to do something for the Connecticut moms and kids with breast cancer, but that *something* quickly morphed into a nonprofit effort to help break through barriers in the lives of moms with MBC. Laser focused on single moms with kids under 19 living at home and financial need, Roberta took her nonprofit (she calls it her fourth child) nationwide in mid-2023 and is already serving women in 27 states. While providing 6 months of financial support to approved applicants remains the core of Infinite Strength, Roberta has added to the support through one-day local (Connecticut) mom-and-kid retreats, in-person and online panels with some of the best experts in cancer care, a 2024 MBC conference, and a groundbreaking effort to change the picture through the Connecticut Coalition of Oncologists. This is a woman who does not sit still and we are so lucky to have her as an ally for people living with MBC. This episode may inspire *you* to get out there and do something!